PNEUMONIA
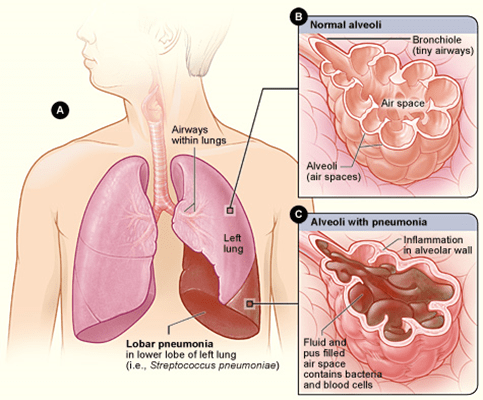
Pneumonia is an infection or inflammation of the lungs. Dogs and cats can develop pneumonia for several reasons, and pneumonia is usually a complication of an underlying problem. Pneumonia often produces generalized symptoms like most other infections in animals: lethargy or tiredness, poor appetite, and so forth. In addition, animals with pneumonia may also develop specific respiratory symptoms as a result of the infection within the lung tissue. These symptoms include shortness of breath, coughing, raspy or fluid-sounding respirations, hacking, and gagging. It is important to know that symptoms may be subtle. It is also important to keep in mind that many disorders other than pneumonia can produce these same symptoms, so a dog or cat cannot be known to have pneumonia, even by the most skilled veterinarian, without diagnostic tests such as radiographs (x-rays) of the chest. Additionally, routine lab tests including a complete blood count, serum biochemistry panel, and urinalysis are necessary to seek out the effects and contributing factors of pneumonia in all animals suspected or confirmed of having pneumonia. Finally, cats with pneumonia should be s tested for feline leukaemia and feline immunodeficiency virus, since these serious conditions can have significantly compromised an animal’s immune system, making pneumonia extremely difficult to treat. The best way to identify specific bacteria involved in pneumonia is to sample them directly, which is done either via transtracheal wash (under sedation, the patient has samples of the lung secretions retrieved with fluid and a catheter) or bronchoalveolar lavage (under general anaesthesia, a small camera [endoscope] is passed into the mouth and down to the lungs to identify and retrieve lung secretions and cells). The following are a few classes of underlying causes of pneumonia: Viral infections: As in people, these are viruses that are passed from one dog to another or one cat to another. Viral infections of the airways typically do not cause pneumonia by themselves but do weaken the local defenses, allowing bacteria to multiply and cause pneumonia. Some viral infections cannot be cleared by the immune system, and these may cause recurrent or persistent problems, whereas others are self-limiting and improve or disappear altogether in a week or two. Megaoesophagus: Weakness of the oesophagus (the tube through which food travels from the mouth to the stomach during swallowing) can lead to recurrent regurgitation or “burping up” of food and water. Under these circumstances, food and water risk being inhaled into the lungs, causing pneumonia. Fungal: Fungal pneumonias are the result of inhalation of spores of fungi in the soil. Examples are coccidioidomycosis (arid parts of the United States and Central America), histoplasmosis, and blastomycosis (damp, moist environments in North America). These fungal infections can cause severe pneumonias that are initially difficult to treat. However, when caught early and with good treatment response by the patient, a complete cure can be achieved. Foreign Material: Foreign material inhaled into the lungs can mechanically and chemically irritate the lungs. The following inflammation often allows secondary bacterial infection and pneumonia. LIVING WITH THE DIAGNOSIS When medical tests, including chest x-rays in every case, confirm that pneumonia is present, treatment is necessary. In milder cases, this may mean antibiotic pills that you can give at home, but if the pneumonia is moderate or severe in degree, the dog or cat generally needs to be hospitalized so the antibiotics can be given by injection and in order to give intravenous (IV) fluids and other medications, as necessary. Another in-hospital treatment commonly used for pneumonia is nebulization, which is the inhalation of highly humidified air to help break up the thick secretions and mucus that are involved in the immune response. Coupage is a technique of gently thumping the chest to help break up the fluid in the lungs’ small airways to allow them to be coughed up. There are other treatments involved in hospitalized care of pneumonia patients, such as oxygen supplementation and ventilatory support, which may or may not be necessary depending on your pet’s specific type and severity of pneumonia. Any pet that has pneumonia needs adequate time for rest and recovery. Often a pet will feel better soon after the initiation of the appropriate supportive care and medications. However, their lungs may still be congested with infected material. They may tire quickly or have shortness of breath after limited activity and can easily do too much. Therefore, any pneumonia patient who is recovering well should still be handled carefully for at least 1 or 2 weeks after symptoms have disappeared to allow the lung tissues to heal adequately. The long-term outlook for recovery (prognosis) is dependent on the severity of the pneumonia and the underlying cause. Bacterial pneumonias are generally rewarding to treat, since a good response to antibiotics results in disappearance of the infection. However, bacterial pneumonia is often the “tip of the iceberg,” since certain viruses (e.g., distemper), concurrent conditions such as megaoesophagus, or other predisposing causes as discussed above are usually present, too, and these may or may not be easy to eliminate. If the underlying cause of pneumonia is curable, then the healing of lung tissue can take place over the following days to weeks. If the underlying cause is not curable (such as scar tissue in the lungs, idiopathic megaoesophagus, etc.), then periodic flare-ups of bacterial pneumonia may occur for the remainder of the animal’s life. The lungs have a great ability to compensate for damage, destruction, and temporary dysfunction. However, in the most severe cases, scarring and secondary damage following pneumonia can be severe enough to cause long-term respiratory (breathing) compromise. Contagion (spread to other dogs or cats) can happen if the underlying cause of the pneumonia is a virus or certain bacteria. This is an important point worth raising with your veterinarian, and here again, the importance of identifying underlying causes of pneumonia becomes apparent. If in doubt, you should avoid having your pet with pneumonia be in contact with other pets to eliminate the risk of direct transmission of viruses or bacteria through secretions or through
Domiciliary (HOURLY) care
Domiciliary (HOURLY) care What is domiciliary care? Domiciliary care — also known as hourly care — involves a care assistant visiting you in your home, supporting your daily needs and enabling you to maintain your independence. With this kind of help, you can continue to live in your own home, keeping to your familiar routine and doing those things you enjoy. Domiciliary care is generally provided for a minimum of 30 minutes and up to as many hours as you need. Carers can rotate, if required, and can visit you as many times as you choose – daily or weekly. Call Us MAKE AN ENQUIRY The benefits of ENA domiciliary care Visits from a domiciliary carer help you to keep your independence and enable you to maintain control over your life. A domiciliary carer can help with multiple household tasks, from meal preparation to cleaning, whilst providing companionship and emotional support when you need it. We take great pride in our domiciliary care service, developed in addition to our live-in care. We guarantee a reliable, professional and dependable domiciliary care service at all times. Simply The Best Lorem ipsum dolor sit amet, consectetur adipiscing elit. Curabitur laoreet cursus volutpat. Aliquam sit amet ligula et justo tincidunt laoreet non vitae lorem. Aliquam porttitor tellus enim, eget commodo augue porta ut. Maecenas lobortis ligula vel tellus sagittis ullamcorperv vestibulum pellentesque cursutu. 10.04.2018 Easy To Use Lorem ipsum dolor sit amet, consectetur adipiscing elit. Curabitur laoreet cursus volutpat. Aliquam sit amet ligula et justo tincidunt laoreet non vitae lorem. Aliquam porttitor tellus enim, eget commodo augue porta ut. Maecenas lobortis ligula vel tellus sagittis ullamcorperv vestibulum pellentesque cursutu. 5 Month Ago Lorem ipsum dolor sit amet, consectetur adipiscing elit. Curabitur laoreet cursus volutpat. Aliquam sit amet ligula et justo tincidunt laoreet non vitae lorem. Aliquam porttitor tellus enim, eget commodo augue porta ut. Maecenas lobortis ligula vel tellus sagittis ullamcorperv vestibulum pellentesque cursutu. 6 Month Ago Why choose a domiciliary care from UNIICARE COMPLEX CARE SPECIALIST ? We’ve been providing domiciliary care since 2009, so we understand exactly what’s required of a domiciliary carer. We know how important it is to maintain independence at home and with the right care in place you can continue to live freely for years to come — a key value upon which the UNIICARE COMPLEX CARE SPECIALIST was founded. We understand that inviting a domiciliary carer into your home might seem daunting at first, but we’ll work to find the right carer for you. We’ll support you through the whole process, matching you with a carer you’ll feel completely comfortable with — someone who understands your routine and your individual needs and above all, is compassionate. With our extensive experience, unrivalled professional and emotional support, and range of care options, the level of service provided by our staff is clearly evident. As care visits will often involve help with tasks such as washing, dressing and taking medication, we know that reliability and consistency is essential and that you depend on our carers to help maintain your quality of life. If you choose to benefit from our domiciliary care service, we guarantee you’ll receive: A highly-trained domiciliary carer A dedicated care coordinator A flexible and reliable care service Care that aims to exceed the guidelines recommended by the CQC Expert advice and support from a friendly, compassionate and professional admin team A 24/7 rapid response service, where required We are Care Quality Commission (CQC) registered and the high quality of our services, along with what you can expect from us, are reflected in our CQC reports. Our CQC provider ID for ENA Hourly Care is 1-4857621816. Did you know — over 80% of our clients have been referred to us by friends or family. We are hugely grateful for this recognition and are continually developing our services and training to improve the level of care we offer. Key elements of UNIICARE COMPLEX CARE SPECIALIST Highly-trained care assistants We hold high expectations of our domiciliary carers — expectations which must be met before joining our team. With value-based interviewing and key criteria, we can ensure candidates are a perfect match for our high standards. Rigorous recruitment processes, thorough background checks and on-the-job supervision further guarantee the calibre of our staff. Guaranteed care cover Our 24/7 care helpline is in place to support our clients and carers outside of office hours. This service offers a qualified care team who can be called upon at short notice, should an emergency ever arise. Expert care and advice Our team has a combined experience of over thirty years in the domiciliary care industry and, as such, we are well-equipped to manage your care needs. Working with other health professionals such as social workers, GPs and therapists, we do everything we can to support the delivery of the best possible health outcomes. We have access to a unique support network of experts in the domiciliary care industry and, if ever there’s something we can’t help you with, we will be happy to refer you to a relevant professional who can. We are constantly striving to use best practice and improvement techniques in the provision we offer. How much does domiciliary care cost? The cost of a domiciliary carer will depend on a number of factors, including how many hours are needed, and whether the care is for yourself or as part of a couple. As a guide, costs for our domiciliary care services start from: £27.00 per hour — Monday to Sunday, exclusive of bank holidays. £21.00 per half an hour — Monday to Sunday, exclusive of bank holidays. We currently provide domiciliary care in Welwyn Garden City, Welwyn, St Albans, Hatfield, Harpenden and surrounding villages. Talk to us about your care needs To talk about your care needs, contact one of our friendly team members Call Us MAKE AN ENQUIRY
Back Pain: A Nuisance to Good Health

Background Back pain is an extremely common complaint. An estimated 80% of people in the UK are affected at some time in their lives. It is also one of the main reasons for sickness absence. On daily average, about 1% of the working age population are on sickness absence due to a back problem. Nearly 5 million working days were lost through bad backs in 2003/04. On average each person affected took about 20 days off in that period. Most back pain is caused by strains and minor injury rather than serious injury and is often called “simple back pain“. Although the pain often comes suddenly and may be triggered by a particular movement, the causes may have been building for some time. Some of the commonest causes of stress and strain on the spine are: On-going poor posture Slouching in chairs Driving in hunched positions Standing badly Lifting incorrectly Sleeping on sagging mattresses Posture Good Posture encourages your muscles, joints and ligaments to work as nature intended. Remember that many adults with chronic back pain can trace their problem to years of bad posture habits. Avoid slouching and stooping. To encourage good posture, try and think about the way you sit and stand. When standing for long periods of time, consider whether your shoulders are hunched; if so, stretch them back gently. Remember that placing pressure unevenly on one leg throws your spine’s curvature, which can make the shoulders and hips uneven. Measures to Reduce Injuring Spine Whenever possible: Avoid lifting and carrying heavy objects. Use a shallow trolley at the supermarket to avoid stooping and bending. Avoid spending long periods of time hunched over the computer. Adjust the car seat to provide you with support and a good position. Take breaks on a long journey; take time to stretch your spine and limbs. Gardening can be a good form of exercise but try not to get too hot or cold as this can increase body stress, due to excessive bending and twisting. Maintain a regular exercise programme. Walking and swimming can contribute to reducing back pain. Activities and Exercises to improve Healthy Spine Muscle Strengthen the muscles that support your spine Improve balance and posture Counter the effects of depression Help you become more flexible and supple Improve circulation Help keep your weight under control Help you sleep better and be more alert mentally Improve your general level of fitness and stamina
Engaging Stroke Recovery Activities

Stroke recovery activities are an important part of regaining your abilities as far as possible following a stroke. Recovering after a stroke is a challenging process. Everyone who has a stroke is affected differently, which means it’s hard to predict how long or successful the rehabilitation process might be. The most common effects of a stroke include: Partial paralysis (usually on one side of your body) Visual problems Altered mood Memory loss Your doctor will recommend a programme of occupational therapy and physiotherapy adapted to your specific needs. These exercises and activities are designed to help you regain as much of your physical and cognitive ability as is feasible. However, depending on your condition, you may also want to supplement these with some additional options that fit with your hobbies and interests. Ideas for additional stroke recovery activities This list contains a range of ideas for people of differing abilities that can supplement the stroke rehabilitation process. Remember, this process is different for everyone; you should only attempt stroke recovery activities you feel comfortable and sufficiently supported in engaging with. And, you should always follow the recommendations of your doctor. 1. Writing and reading Penning letters to friends or relatives, writing stories and memoirs, or just getting lost in the pages of a good book; these are all productive and enjoyable things to do while recovering from a stroke. Writing and reading are great ways to stay occupied and develop a sense of accomplishment, even when you’re not able to live as you did before. They can also help to improve your dexterity. 2. Cooking With safety in mind, you could try improving your cooking skills during stroke recovery. Cooking is a great independent or shared activity, with a tasty outcome that you can enjoy with loved ones. It’ll also enhance your understanding of your nutritional intake, enabling you to adopt a diet that’s beneficial for stroke rehabilitation. 3. Music Playing an instrument, or simply listening to your favourite music, are relaxing activities that are known to have a positive effect on mood. Handling an instrument is one way of improving your coordination. Or, you could combine listening to music with a spot of light dancing to introduce an element of exercise. 4. Arts and crafts Arts and crafts will engage your brain as well as your hands, helping you become more precise with your movements. Choose your creative outlet; it could be woodwork, paper crafts, glass/ceramic work – even flower arranging. Each has its own unique benefits and appeal. 5. Gentle exercise/physiotherapy Gentle exercise and physiotherapy will help you regain muscle and movement capacity, as well as aiding your overall health. Follow your doctor’s advice (they’re likely to recommend different activities for different stages of your recovery). But, also look for other opportunities to get active, such as going for a walk in a local park. 6. Meditation Meditation is an effective way to reduce stress and approach life with added positivity; both of which are immensely important during stroke recovery. This doesn’t have to be a formal process. Just remember to set aside some time to sit quietly each day, focus on your breathing and collect your thoughts. 7. Brain training Whichever technique you choose, brain training includes low-impact yet fun activities suitable for people at most stages of stroke recovery. You could try a puzzle, jigsaw, crossword, sudoku, memory game, board game, or a spot of mental arithmetic depending on your preferences. 8. Days out At a more advanced stage of recovery, you can start to think about planning some local days out. This could give you a change of scenery and an opportunity to interact with friends in your community. Start with short, local trips and build up from there. Make sure you only do as much as you feel comfortable with and have access to the support you need. Getting back on your feet following a stroke can be difficult, but these stroke recovery activities can help make this process more engaging. Speak to our friendly team to find out how.
skills you need to get hired as a Live-In Carer

There is no better option than a career in Live-In Care if you have a natural passion for helping others. As a Live-In Carer, you can experience an unmatched level of professional fulfillment and job satisfaction, providing support at a personalised and sustained level – a quality of care which is sometimes difficult to deliver in a care home or hourly care setting. By choosing a live in care job, you will be making a difference in the lives of a person at a time when they need companionship and support the most. Live-In Care does present its own unique challenges and requires a select set of characteristics to prepare a person for the responsibility of around the clock care in a home environment. Find out whether you possess these top qualities needed to become a successful Live-In Carer. 1. Professional Or Personal Care Experience Having previous experience in Live-In Care is extremely valuable, unlike other care provisions, carers will typically work alone during a placement. This means there is often little opportunity for shadow learning. Although all Live-In Carers will conduct extensive training before being placed with a client, a good understanding of the fundamentals such as manual handling, medication management, and current care delivery techniques will provide a great platform from which further knowledge and Live-In Care specific skills can be built upon. Your knowledge of care can be acquired from both professional experiences developed through a work environment or from personal experience from caring for a loved one or friend. Be sure to highlight any specialist training and qualifications you may have had with complex conditions such as dementia, as these skills demonstrate that you are proficient with dealing with clients with more complex needs and can be given greater responsibility. 2. Availability & Flexibility A Live-In Carers reliability and dependability is a major factor. On the whole, care professionals typically work unusual hours, as a person’s needs do not stop when business hours end – this is especially true for Live-In Carers. A predetermined rota pattern will be worked out before your placement begins, a typical pattern will often have you working consistently for say 2 weeks on before taking a 2-week break, sometimes the rotation can be longer, such as 4 weeks on 2 weeks off. They vary and there are many options to suit your lifestyle. When you are on duty you will work an average number of hours each day, with a 2 hour break during your shift. During your off periods, you will also be asked to vacate the property. In order to provide consistent and familiar care a great deal of availability and flexibility is required, including arranging accommodation during your days off. Before entering a Live-In Care job it is important to consider whether your lifestyle is suitable and if you are able to commit to the rota patterns. 3. Listening & Communication A unique aspect of Live-In Care is the ability to provide companionship alongside needs related support, the combination of these two factors can have amazing effects on a person’s well-being and happiness. Listening to and acknowledging your client’s opinions and wishes as well as respecting their choices is key for building a trusting and enjoyable relationship. A good Live-In Carer will understand how to engage and respond to the person receiving care, show interest and understanding whilst also maintaining a productive care routine throughout the day. Carers may also be asked to accompany a client to doctors and hospital appointments, having the ability to listen carefully and clearly communicate instructions from appointments will be a large part of your role as a carer, therefore you often required to have excellent English speaking and writing skills. 4. Organisation & Planning A Live-In Carer will become responsible for certain aspects of their clients home, this can include anything from the preparation and cooking of nutritional meals to completing household chores. Ensuring the home environment is clean, safe and comfortable is as equally part of a Live-In Carers role as delivering the care plan. Live-In Care gives people the ability to remain independent in their homes, therefore you may be asked for assistance with simple administration tasks such as paying bills, posting letters, or helping your client attend classes and activities in the community. In order to keep the household running smoothly, tasks will need to be overseen with prior preparation, scheduling, and planning. 5. A Caring Nature There’s no denying that care in any form is difficult, as it requires you to put another’s needs and considerations before your own. There are particular personality traits believed to indicate whether a person will adapt well to the responsibility and challenges of Live-In Care-taking it in their stride. These characteristics include: Patience – Having the ability to calmly and coolly handle situations that arise during care without becoming frustrated is vital. Empathetic and understanding – Recognising and demonstrating compassion for your client and their loved ones, always putting yourself in their shoes Sensitive – As a Live-In Carer you must be in tune with your client’s wellbeing, and have the ability to provide care with dignity in all situations. Supportive – A Live-In Carers role is to aid the person in continuing their independence at home, assisting your client with their wishes and choices. Responsible and Resilient – A good Live-In Carer will be able to deliver the care plan in a professional manner and show resilience and creativity when the care doesn’t always go to plan! As a growing number of people choose to stay at home whilst receiving care, the need for fantastic Live-In Carers is at an all-time high. As a Live-In Carer, there is a great deal of opportunity for you to develop, improving the service you provide as you continue to discover new aspects of your client’s personality and preferences, as well as building a bond which is valued by both you and the person you deliver care to. With excellent support, extensive training and generous benefits, a career in Live-In Care can be extremely beneficial
What does ‘independence’ mean to older people?

Independence is a simple concept. At its most basic level, it means having full autonomy over one’s own life. However, the challenges posed by the ageing process can challenge this definition, especially when it is clear that assistance is needed to perform daily tasks. Throughout our adult lives, most of us are able to determine our own actions and decisions, but as we reach our older years, the scope of our independence can diminish as a result of changing mobility or health. However, with the right care package in place, your loved one can enjoy as much independence as possible whilst also receiving the support they need. How to nurture older people’s sense of independence A person’s desire to remain independent is not always reflected in their capabilities, and this conflict can become increasingly pronounced as time goes by. Giving your loved one as much input as possible in the decisions that affect them can benefit them emotionally and physically, as well as giving them a higher quality of life. Here are some ways you can help your loved one feel more independent: Decision-making At the heart of independence is the ability to make decisions for yourself. Older people are accustomed to deciding their own actions, and removing this sense of self-determination can lead to feelings of denial and depression. Here are some key factors to consider when it comes to decision-making: Don’t assume that a person is unable to make a decision for themselves Encourage them to make healthy life choices by presenting them with relevant information and asking their opinion on major decisions, especially those that concern them Choice and control can help older people maintain their existing skills Empowerment To facilitate the decision-making process, you will need to take steps to empower your loved one. This will require you to: Dedicate enough time for them to make a decision, and for the choice to be facilitated Give them an active role in arranging engaging activities Know how to facilitate a decision in a safe and appropriate manner Reassure them that the choice is theirs to make In practice When a person’s ability changes, it’s easy to overlook some of the choices that feed into their sense of independence. These are some of the ways you can make sure you’re promoting independence in practice: Encourage them to do as much as they are able. If they can no longer perform a whole task, let them to do what they can before assisting with what’s left Involve them in everyday decisions, like choosing their own meals or social activities Give them as much agency as possible in larger decisions, such as care options or adaptations to the home Familiarise yourself with their life story, so that you can help them draw on their past experiences to inform current choices 97% of people would prefer to live the rest of their lives in their own homes, rather than move into residential care. If this is what your loved one decides they want, live-in care will enable them to stay in the familiar and welcoming environment of their own home, supported by a team of two carers who are present 24/7. If you would like to explore how live-in care can help your loved one safely maintain maximum independence in their later years, please feel welcome to contact us by email: info@unicarerecruit,co.uk or by phone 0208 239 6877 for an exploratory discussion.
Signs of Real Hope

After months and months of restrictions, continued uncertainty around work, education and our general health, and the shared anxiety about the future course of this pandemic, we are now in the unusual position of receiving some cautiously optimistic news. Subject to stringent safety checks, Medicines and Healthcare Regulatory Agency (MHRA) approval, Joint Committee on Vaccination and Immunisation (JCVI) advice, product availability, and the diligent oversight of NHS England and Improvement and Public Health England – a new COVID-19 vaccine could be ready for distribution in modest amounts before Christmas. Larger quantities of vaccines may be available in the first half of 2021. Of course, this news – though welcome – comes too late to take the edge off the challenging winter our amazing health and care professionals will undoubtedly face, but it does offer some hope for better times ahead. Coronavirus has had a particular impact on the social care sector and the people it protects, supports and sustains. Many thousands of care staff have juggled caring responsibilities for families, friends and loved ones with providing care and support to people most at risk from this dangerous disease. At times, they have succumbed to the virus themselves or been obliged to self-isolate to keep others safe. The mental and physical toll has been huge. We thank them all for their tireless dedication, kindness and compassion each and every day. I hope it is reassuring that the JCVI’s interim advice on prioritisation recommends that a vaccine should first be given to care home staff and residents as the highest priority if practical to do so. This advice sets out that vaccinations should then be prioritised according to final JCVI advice. Health and social workers will be part of this prioritisation. This advice is of course regularly reviewed and subject to change. Assuming vaccinations can begin soon, it will be a huge undertaking. That said, I know our sector partners, local authorities and health and care services will do all they can to make distribution, access and application as smooth and stress free as possible. Maintaining the highest safety standards In the meantime, all care providers – those running care homes in particular – will be making sure PPE supplies, testing regimes and all relevant infection control measures continue to be observed to keep residents, staff and visitors safe. On that point, the recently announced visitor testing programme should give added hope and peace of mind to care staff, residents and families who will all, at times, have felt the distress and discomfort caused by current restrictions, especially for those living with dementia or approaching end of life. This is also a crucial point. As with flu vaccinations and testing, legislation and guidance is in place to make sure the best interests of people without capacity are respected. Such decisions must always involve the individual, family members and those closest to them, not just health and care professionals. We will continue to speak with stakeholders, health and care experts, and people with lived experience to make sure we get this right. It’s about more than just vaccines More generally, as we hope to cascade vaccinations through the population, we recognise people are not simply defined by categories and age groups. With or without a vaccine, we all have a vital role to play in protecting our own health and likewise the health of those around us. We must all recognise, encourage and inform each other of the need to minimise risk factors in our daily lives. For those receiving care, we also know their needs are bespoke. There cannot be a ‘one stop shop’ approach to administering the vaccine to everyone. A jab may be appropriate for some, but not for others. Clearly, there are logistical, clinical and policy challenges to overcome, but I am confident our sense of shared endeavour will make sure that we do. Whatever happens, we will keep engaging with the sector, testing our advice and acting on feedback. These vaccines may represent the most positive news in months, but it is still the kindness, compassion and dedication of our health and care professionals that will really see us through this pandemic and beyond. Source: gov.uk
Smoking Kills

SMOKING KILLS, UK GOVERNMENT PLANS TO ENSURE SMOKEFREE SOCIETY BY 2030 Smoking causes nearly 1 in 5 cancer cases and more than 1 in 4 cancer deaths each year in the UK. Decades of policy action have steadily cut the UK’s smoking rates to one of the lowest in Europe. But with around 1 in 7 people still smoking, tobacco continues to place an enormous cost on our society and our economy. Last November, the UK Government published its vision to put “Prevention at The Heart of Our Nation’s Health”, recognising the importance of preventing cancer amongst other long-term health conditions. A government policy published, gave an indication of some new and old ways that the Government might deliver on this. And when it comes to tackling smoking, the plan to make England “SMOKEFREE” by 2030 is bold. The government is on high priority alert to make smoking become a thing of the past. The MPs are working assiduously with government to achieve this intended purpose of contributing towards the United Nations Sustainability Development Goal 3 of attaining Good Health and Wellbeing for its citizens. To achieve this milestone of ensuring smoke free environment, the leadership have made personal and moral commitment to contribute effectively to bring to finality the intended purpose of achieving this aim of “SMOKEFREE” environment in England by the end of the next decade. NHS And Local Government Need Support NHS England has promised that, by 2024, every hospital patient who smokes will be offered treatment to help them quit. But this is not enough. People also need to be offered treatment to quit by their General Practitioners. Smoking cessation services in local communities are being increasingly threatened. The Government must support local councils and authorities with funding to help them pay for vital services that are proven to bring smoking rates down. Slashed budgets have jeopardised vital public health services. And since 2015, the public health budget has fallen by £700 million. Funding for wider tobacco control measures and stop smoking services have been among the worst hit. The NHS must liaise with “Stop Smoking Services” which offer smokers a combination of pharmacotherapy and behavioural support. These are thoughtful ways of providing support for numerous patients who are ready to quit smoking. However, ongoing cuts to public health funding have meant that just over half the local authorities in England have a specialist stop smoking service open to all smokers in the area. Possibility of a ‘Polluter Pays’ Approach Tobacco companies are responsible for the greatest and most enduring man-made public health epidemic in history, yet they continue to profit from a product that kills one in two people who use it. In its Policy Paper, the Government recognises that charging tobacco companies in France and the USA for the damage they cause has helped to fund some tobacco control efforts, suggesting that the UK may be open to a similar approach. These new Government proposals mention a charge on the tobacco industry. This is something the government has tabled since 2015. It is part of a potential solution to plug the current funding gap for tobacco control. More than 7 in 10 adults in England said they would support a fee on tobacco manufacturers that could fund stop smoking services and prevent young people from taking up smoking, according to reports commissioned by Action on Smoking and Health (ASH). It is a matter of fairness that the tobacco industry should pay for the damage to health that they have caused says the Government. Alongside this, the Policy paper also suggests that an “Insert carrying quitting advice” could be included inside cigarette packs. Canada is the only country in the world that does this, the government hope this could discourage young adult smokers from continuing to smoke. Organisations and companies with an interest in the proposed measures – whether they prioritise public health or not – are now free to weigh to influence how these proposals are taken forward.
Living with Dementia During the Christmas Period

Christmas can be a very exciting time for many of us. Exchanging gifts, spending quality time with your nearest and dearest and trying to make it all the way through Christmas dinner without dropping your paper hat in the gravy; it truly can be the most wonderful time of the year. Not only that, but it’s traditionally a time for hope and spreading joy; being together as a family and celebrating everything that is good in the world. But for some, Christmas isn’t always a time for joy and excitement; it can bring back painful memories of loved ones that are no longer with us, which can be particularly confusing and frightening for someone living with dementia. We already know that Christmas is probably going to be very different for us all this year, but if your loved one has dementia, there may be a few scenarios that could make them feel a little unsettled. Here are a few small adaptations you can make this Christmas to make your festive season dementia friendly. Decorate gradually Transforming your home into a festive fantasy overnight may cause your loved one to feel a little confused, especially if some parts of your house are a little less recognisable. Perhaps try and put the decorations up gradually over the course of a few days and ask your loved one to help. That way, they can feel more involved and be a part of the Christmas process. Keep food portions small Dementia can have a big impact on appetite, which can lead to those living with dementia feeling intimidated if their plate is filled with food. Be mindful of portion sizes, and perhaps try a few vegetables and a slice of meat to start with – your loved one can always go back for seconds! Create a safe space Christmas activities can bring a wealth of joy and laughter, but if your loved one starts to feel a little unsettled by the noise, it may help to find a safe space for them to go and be in the quiet for a little while. If you can, try to keep a quiet room free for them, in case they become overwhelmed and need a little break. Bring a little nostalgia It may be that you have photographs to share from Christmases past, or perhaps you have your loved one’s favourite Christmas album on CD or available to stream. Revisiting happy memories will bring some familiarity for your loved one, subsequently helping them to feel more at ease. Acknowledging the past It’s also important to be open to discussing why Christmas might be particularly difficult for them if their loved ones are no longer here, or if they just don’t like Christmas in general. Gently help them remember good times with those that have passed by discussing any fond memories you have of them. Keep them involved Dementia can be a very lonely condition to live with, and feeling confused or unsettled in a room full of people might lead them to feel quite isolated. If you can, be mindful to involve your loved one in games and conversation; it might well be the thing that helps them to relax throughout the day. An alternative to Christmas Some people just don’t like Christmas, and that could be exactly how your loved one has felt all of their life before they had dementia. Why not ask them how they want to spend the day? They might not want to put up any decorations but instead just want to enjoy a cooked dinner and some peace and quiet. Be mindful that although you may love Christmas and the weeks leading up to it, it might not hold the same sentiment for them. If you or your loved one would like additional support this Christmas, we’re here to help. Our care teams work right through the Christmas and New Year period and are available to support with hourly visits or 24-hour live-in care. Whether it’s help with getting dressed and ready for your family festivities or simply a friendly face to pop in and spend some quiet time with you, our dedicated team of carers are here to support you this Christmas. We can also support families in different areas to meet up with one another if you live a fair distance away from your loved one. Get in touch with us today to discuss your needs in more detail.
The relationship between music and dementia

Dementia can have a tremendous impact on the person living with it, but also their family and loved ones. There are many types of dementia, including Alzheimer’s and vascular dementia, and the symptoms differ between each type. However, because dementia affects the brain, one of the most common symptoms is noticeable memory loss and having difficulty with tasks that they could do with ease before their diagnosis. There are many different techniques that you can use to alleviate the symptoms of dementia, which can help ease the challenges faced by someone who is living with the condition, and those closest to them. It has been found that music can have an influence on dementia, it can work towards ‘unlocking’ memories and reaching parts of the brain which other forms of communication cannot. Using music within dementia care Music can be an incredibly useful tool when caring for someone living with dementia. It can help to calm someone, change their mood, connect with others and even reduce the feelings of isolation often associated with dementia. Playing soothing or familiar music can result in an emotional reaction, which can be explained through the initial development of the brain. “We know that the auditory system of the brain is the first to fully function at 16 weeks, which means that you are musically receptive long before anything else,” explains Professor Paul Robertson, a concert violinist who later went on to study the connection between music and dementia. “So, it’s a case of first in last out when it comes to a dementia-type breakdown of memory.” This means that someone with dementia loses their most recent memories first, and they remember their oldest memories most strongly. To start, you could try playing your loved one a song that once meant a lot to them. This could be the music they had their first dance to, a favourite song from their youth, or one that might remind them of a special occasion. It is important to remember to watch their reaction as the music plays. If they appear to be uncomfortable or agitated, turn the music off. It could be down to something as simple as the wrong song choice, or perhaps they are not in the right frame of mind, so try it again at a later time with another genre of music or a different time of day. As research shows, using music when caring for an individual with dementia can not only help the individual to feel genuinely relaxed and comforted, but it can also help you to understand the progression of their condition and what makes them feel happy. Here at Unicare, we believe that dementia care at home can provide you and your loved ones with the tools you need to live comfortably at home, with more time to spend together as a family. Whether you think they’d benefit from some companionship, or perhaps your loved one would like some support getting out of the house, our person-centred care is tailored around you and your needs. For more information, please call 0208 239 6877 or email us at info@unicarerecruit.co.uk and we will call you.
